Overview
Your gut microbiome is your inner garden—the more good bugs you have in it, the more likely it is to flourish. Our gut bacteria regulate many bodily functions, from creating vitamins to controlling our immune system, brain function, and, of course, our metabolism and weight. They are critical to our long-term health. But even if you’re eating the right things, you may need outside assistance to maintain plentiful and diverse gut bacteria. Probiotics help populate your gut with beneficial bacteria, improving your sleep, daily elimination, brain health, and so much more.
On today’s episode of The Doctor’s Farmacy, I’m excited to talk to Raja Dhir about the gut microbiome's important role in our overall health, its connection to various diseases, and what can be done to fix our gut. We start our conversation by reviewing the specific ways our gut microbiome influences our health and its connection to autoimmune and neurodegenerative diseases, mood disorders, heart disease, diabetes, and cancer. Raja also shares the three main drivers of microbiome health: what you eat, the medications you take, and your lifestyle.
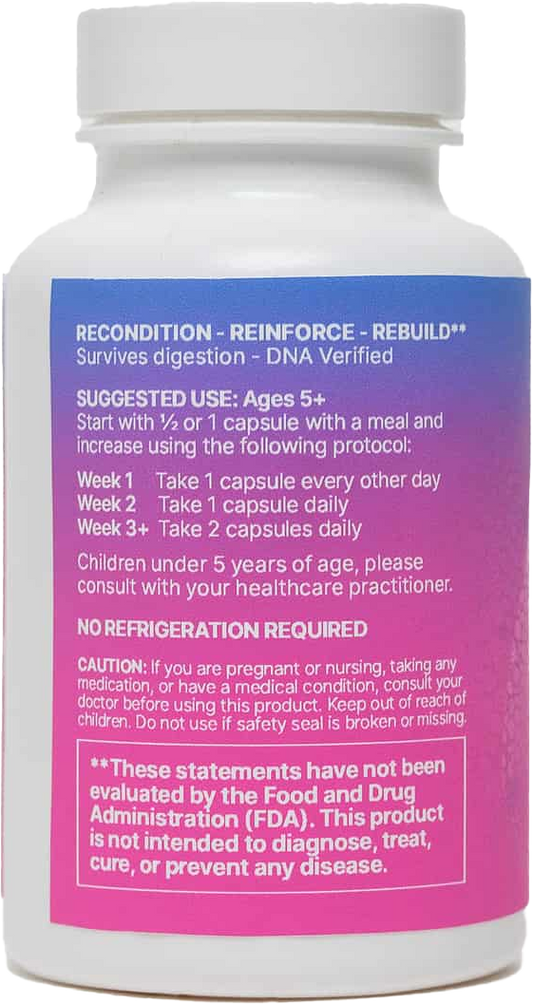
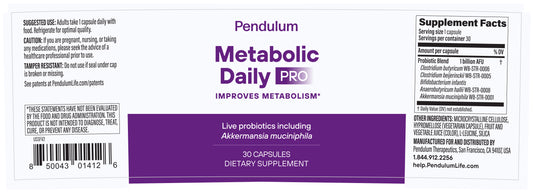
We dive deep into akkermansia, a bacteria I’ve been very interested in since using it to heal my gut several years ago. Raja explains how to get the most out of taking akkermansia and the surprising effect it can have when eating a diet of ultra-processed foods. Raja also shares his thoughts on the explosion of research on the gut microbiome, the need for a deeper understanding of the microbiome in medical practice, and the challenges in navigating the complex field. Probiotics have gained immense popularity for supporting the microbiome. However, there’s also confusion and misinformation about them. We discuss what probiotics are, whether or not we should be taking them, and the importance of purity, potency, and efficacy when choosing a probiotic.
Raja shares insights into Seed’s approach to probiotics, including using a broad spectrum consortium of bacteria. Raja also talks about the impact that antibiotics have on the gut microbiome and the potential benefits of using probiotics to support your body after using antibiotics. We are in an era of discovery when it comes to the gut microbiome and its connection to our overall health, and this is a fascinating conversation that you won’t want to miss!