1 Minute to Change the Future of Medicine
In one minute you can change the future of health care, and have an enormous impact on reducing our chronic lifestyle driven disease burden that accounts for 84 percent of our $3.8 trillion annual health care bill.
Click the link below now and sign the petition for the ENRICH ACT (Expanding Nutrition's Role in Curricula and Healthcare (ENRICH) Act, co-sponsored by Reps. Tim Ryan (D-Ohio) and Pat Tiberi (R-Ohio), to fund nutrition and physical activity training for doctors in medical school. The funds will come from an existing pool of money and therefore, require no “extra” spending or extra cost the taxpayer.
With one click you can start a domino effect that will address the simple fact that most chronic diseases (heart disease, type 2 diabetes, cancer, dementia, autoimmune disease, and more) are caused by food, and can be prevented, treated and often reversed by food, yet doctors learn nothing about food in medical school.
Please stop and sign it now! It costs you nothing, but can change everything.
Petition Link: http://action.timryanforcongress.com/page/s/enrich-act
A few weeks ago I made a trip to Washington, DC to help my friend Congressman Tim Ryan introduce the bipartisan ENRICH ACT into Congress. We briefed other Congressman and Senators and their aides, Republican and Democrat. Everyone was supportive and understood the importance of training doctors in lifestyle and nutrition.
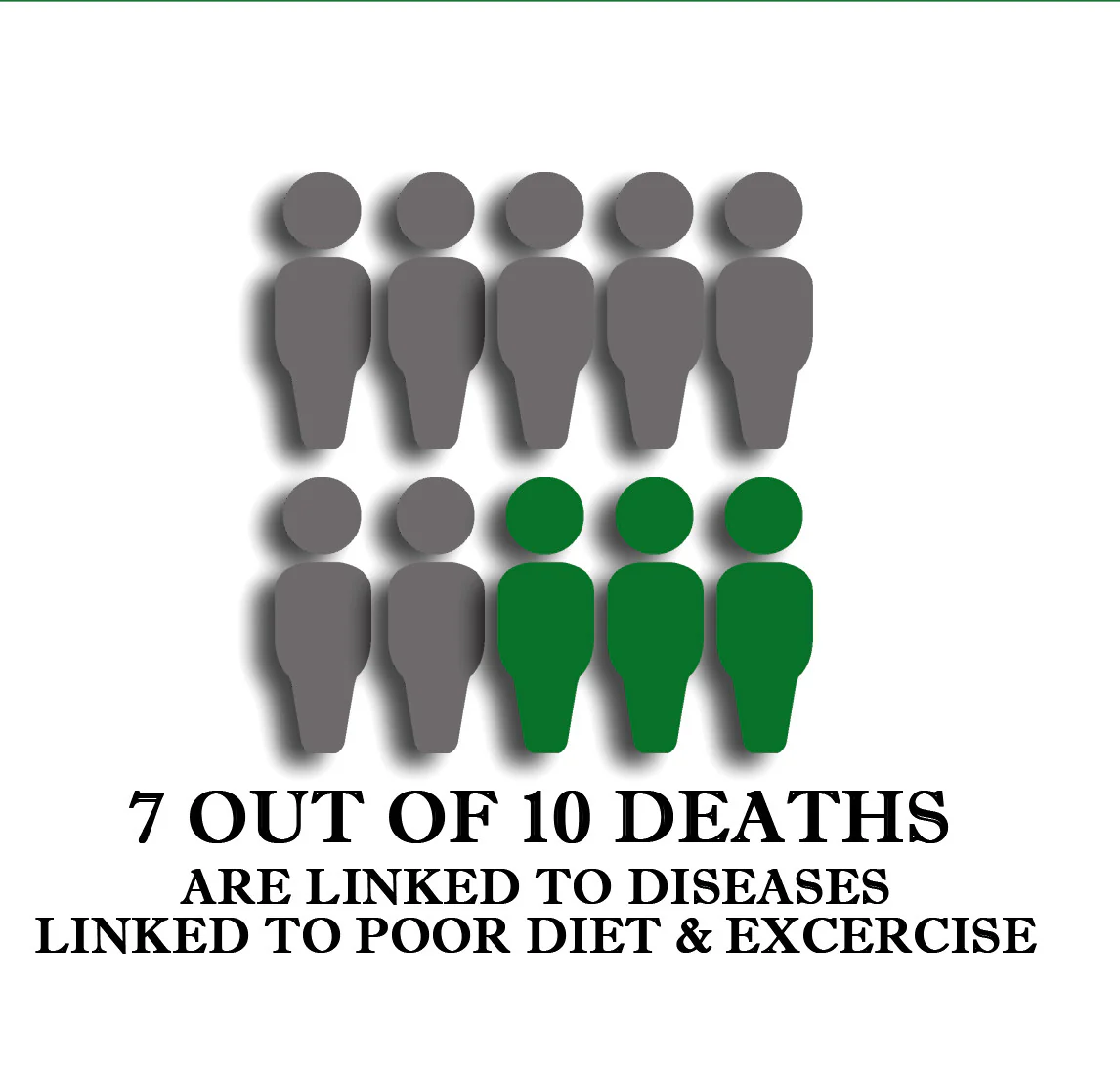
We must start to address the causes of our health care crisis and chronic disease epidemic that afflicts one in two Americans. Obesity and type 2 diabetes – what I call “diabesity” – affect one in two Americans, and one in four children, and alone will cost $10 trillion over the next 10 years. Type 2 diabetes, which can be prevented and often reversed by food accounts for one in three Medicare dollars.
The former Secretaries of the US Department of Agriculture and Health and Human Services, along with the Bipartisan Policy Center wrote a clear impassioned blog on why changing medical school education is a simple, yet powerful lever for change.
The human and economic costs of lifestyle caused disease have wide ranging risks to us as a society. if we do not reverse this trend, this lifestyle will result in premature death and disability, and affect our national security because military recruits are not fit to fight, our global competitiveness due to the “achievement gap” because our children are too sick to learn, and our economic security because Medicare and Medicaid costs will consume 100 percent of federal tax revenue by 2042.
How will we change this?
We must address this through multi-dimensional efforts that change our food system, the quality and type of food we produce and consume access to healthy food, innovative policies, as well as changes in our environment and in our health care system. And we need to help doctors use food as medicine, which often works faster, is better and is cheaper for treating chronic disease than conventional medication or surgery.
Addressing these problems sometimes seems overwhelming but the ENRICH Act provides a simple strategy that can have wide ranging impact.
The ENRICH Act would establish a $15 million competitive grant program administered through the Health Resources and Services Administration (HRSA) in coordination with the NIH National Heart, Lung, and Blood Institute (NHLBI) for medical schools to integrate nutrition education and physical activity into their curricula.
Medical school education needs to change. Consider these facts:
- A 1985 National Academy of Sciences (NAS) report recommended that all medical schools require at least 25 contact hours of nutrition education.
- In 2004, only 38 percent of medical schools met these minimum standards by requiring 25 hours of nutrition education as part of their general curricula. By 2010, that numberhad shrunk to 27 percent.
- Over half of medical students feel their nutrition education is inadequate.
- Current data indicate that few residents, fellows, and other clinicians are comfortable with managing their patients’ nutrition problems.
- Only 13.8 percent of physician office visits included counseling about nutrition or diet and only 12.3 percent included physical activity for patients diagnosed with a chronic health condition.
- 94 percent of physicians feel that nutrition counseling should be part of primary care visits, but only 14 percent feel qualified to offer it.
How will the ENRICH Act address this:
- At least 10 grants totaling $5 million per year for three years will go to medical schools, and would fund at minimum of 30 medical schools.
- Grants will target medical schools that combine nutrition and physical activity education with residency programs, help medical schools meet the NAS standard of providing at least 25 hours of nutrition education, and support medical schools that integrate a comprehensive nutrition curriculum that includes physical activity with other health care professional education programs.
- HRSA will submit annual reports and a final report to Congress evaluating the ENRICH grant program and establish best practices for improving nutrition education among physicians.
We often feel powerless to create real change. Once in a while a chance comes along to make a real difference. Now is that time.
Please stop and sign the petition now! It costs you nothing, but can change everything.
Petition Link: http://action.timryanforcongress.com/page/s/enrich-act
Wishing you health and happiness,
Mark Hyman, MD.
References
- Van Horn L. The Nutrition Academic Award: brief history, overview, and legacy. Am J ClinNutr. 2006;83(suppl):936S–40S.
- Centers for Disease Control and Prevention. Chronic Diseases and Health Promotion. Available at http://www.cdc.gov/chronicdisease/overview/index.htm. Accessed March 18, 2014.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012.JAMA. 2014;31:806-814.
- Ogden, CL., Carroll MD, Curtin LR, et al. Prevalence of High Body Mass Index in U.S. Children and Adolescents, 2007-2008. JAMA. 2010;303:242-249.
- Dietary Guidelines Advisory Committee. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines forAmericans, 2010, to the Secretary of Agriculture and theSecretary of Health and Human Services. Washington, DC:U.S. Department of Agriculture; 2010.
- Adams KM, Kohlmeier MP, Zeisel SH. Nutrition Education in U.S. Medical Schools: Latest Update of a National Survey.Acad Med. 2010;85:1537–1542.
- Adams KM, Kohlmeier MP, Zeisel SH. Nutrition Education in U.S. Medical Schools: Latest Update of a National Survey.Acad Med. 2010;85:1537–1542.
- DeLegge MH, Alger-Mayer S, Van Way III CW, Gramlich L. Specialty Residency Training in Medical Nutrition Education:History and Proposal for Improvement. J ParenterEnteral Nutr.2010;34(suppl):47S-56S.
- Friedman G, Kushner R, Alger-Mayer S, Bistrian B, GramlichL, Marik PE. Proposal for Medical School Nutrition Education:Topics and Recommendations. J Parenter Enteral Nutr.2010;34(suppl):40S-46S.
- Eakin EG, Smith BJ, Bauman AE. Evaluating the population health impact of physical activity interventions in primarycare—are we asking the right questions? J PhysActiv Health.2005;2(2):197–215.9.
- Meriwether RA, Wilcox S, Parra-Medina D. Physical activityinterventions in clinical settings. CurrCardiovasc Risk Reports.2007;1(3):237–246.
- 12. Kreuter MW, Chheda SG, Bull FC. How does physician adviceinfluence
Related Longevity Articles
-
 6 min read
6 min readUnlocking the Secrets of Resistant Starch for Health and Longevity
Diet & Nutrition Longevity -

-

-

-
 8 min read
8 min readFresh Starts and Fast Results: Your 10-Day Plan for the New Year
Diet & Nutrition Longevity -
 9 min read
9 min readAmerica’s New Dietary Guidelines Get the Big Picture Right—and That’s a Big Deal
Diet & Nutrition Longevity -

-

Login
- Choosing a selection results in a full page refresh.
- Opens in a new window.







