Why Women Should Stop Their Cholesterol Lowering Medication

If you are a post-menopausal women with high cholesterol, your doctor will almost certainly recommend cholesterol lowering medication or statins. And it just might kill you. A new study in the Archives of Internal Medicine found that statins increase the risk of getting diabetes by 71 percent in post-menopausal women.
Since diabetes is a major cause of heart disease, this study calls into question current recommendations and guidelines from most professional medical associations and physicians. The recommendation for women to take statins to prevent heart attacks (called primary prevention) may do more harm than good.
Statins have been proven to prevent second heart attacks, but not first heart attacks.
Take it if you already have had one, but beware if your doctor recommends it for you if have never had a heart attack.
This current study adds to an increasing body of literature questioning the benefits of statins, while highlighting their potential risks.
New Study Shows 48 Percent Risk of Diabetes in Women Who Take Statins
This study examined the data from the large government sponsored study called the Women’s Health Initiative, the same study that disabused us of the idea that Premarin prevented heart attacks in postmenopausal women.
In fact, based on this randomized controlled trial, estrogen replacement therapy, once considered the gold standard of medical care for the prevention of heart disease, was relegated to the trash bin of history joining medicine’s many other fallen heroes including DES, Thalidomide, Vioxx, Avandia, and more.
In this new study researchers reviewed the effect of statin prescriptions in a group of 153,840 women without diabetes and with an average age of 63.2 years. About 7 percent of women reported taking statin medication between 1993 and 1996. Today there are many, many more women taking statin medications, thus many more are at risk from harm from statins.
During the 3-year period of the study, 10,242 new cases were reported – a whopping 71 percent increase in risk from women who didn’t take statins. This association stayed strong at a 48 percent increased risk of getting diabetes, even after taking into account age, race/ethnicity, and weight or body mass index. These increases in disease risk were consistent for all statins on the market.
This effect also occurred in those with and without heart disease. Surprisingly disease risk was worse in thin women. Minority women were also disproportionately affected. The risk of diabetes was 49 percent for white women, 57 percent for Hispanic women, and 78 percent for Asian women.
But in a typical “my mind’s made up, don’t confuse me with the facts” statement by the medical establishment, the researchers said we should not change our guidelines for statin use for the primary prevention of heart disease.
In a large meta-analysis published in the Lancet last year, scientists found that statins increased the risk of diabetes by 9 percent. If current guidelines were followed for those who should take statins, and people actually took them (thank God only 50 percent of prescriptions are ever filled by patients), there would be 3 million more diabetics in America. Oops.
Other studies have recently called into question the belief that high cholesterol levels increase your risk of heart disease as you get older. For those over 85 it turns out having high cholesterol will protect you from dying from a heart attack, and, in fact, from death from any cause.
Low Cholesterol May Kill You
A recent study showed that in healthy older persons, high cholesterol levels were associated with lower non-cardiovascular-related mortality. This is extremely concerning because millions of prescriptions are written every day to lower cholesterol in the older population, yet no association has been found between higher cholesterol and heart disease deaths for those aged 55 to 84; and for those over 85, the association seems to be inverse — higher cholesterol predicts lower risk of death from heart disease.
The pharmaceutical industry, medical associations, and academic researchers whose budgets are provided by grants from the pharmaceutical industry continue to preach the wonders of statins, but studies like these should have us look good and hard at our current practices. Are we doing more harm than good?
Cardiologists recommend putting statins in the water and giving them out at fast food restaurants and having them available over the counter. They believe in driving cholesterol as low as possible. Statin prescriptions are handed out with religious fervor, but do they work to prevent heart attacks and death if you haven’t had a heart attack already?
Bottom line: NO! If you want to learn why this is true, read on.
Statins Don’t Work to Prevent First Heart Attacks
Recently, the Cochrane Group did a review of all the major statin studies by an international group of independent scientists. The review failed to show benefit in using statins to prevent heart attacks and death. In addition, many other studies support this and point out the frequent and significant side effects that come with taking these drugs. (i) If scientists found that drinking two glasses of water in the morning prevented heart attacks, even if the evidence was weak, we would jump on board. Big up side, no down side.
But this is not the case with statins. These drugs frequently cause muscle damage, muscle cramps, muscle weakness, muscle aches, exercise intolerance (ii) (even in the absence of pain and elevated CPK – a muscle enzyme), sexual dysfunction, liver and nerve damage and other problems in 10-15 percent of patients who take them. (iii) They can also cause significant cellular, muscle, and nerve injury as well as cell death in the ABSENCE of symptoms. (iv)
There is no lack of research calling into question the benefits of statins. Unfortunately, that research doesn’t get the benefit of billions of dollars of marketing and advertising that statins do. One big trial was touted as proving statins work to prevent heart attacks, but the devil is in the details.
It was the JUPITER (v) trial that showed that lowering LDL (or bad cholesterol) without a reduction in inflammation (measured by C-reactive protein) didn’t prevent heart attacks or death. (vi) Statins happen to reduce inflammation so the study has been touted as proof of the effectiveness of these medications.
Mind you it wasn’t lowering the cholesterol that helped (which is the intended purpose of statins), but the fact that they lower inflammation. What is ignored by people who use this study to “prove” that statins work is the fact that there are so many better ways to lower inflammation than taking these drugs.
Yet other studies have shown no proven benefit for statins in healthy women (vii) with high cholesterol or in anyone over 69 years old. (viii) Some studies even show that aggressive lowering of cholesterol can cause MORE heart disease. The ENHANCE trial showed that aggressive cholesterol treatment with two medications (Zocor and Zetia) lowered cholesterol much more than one drug alone, but led to more arterial plaque and no fewer heart attacks. (ix)
Other research calls into question our focus on LDL or the bad cholesterol. We focus on it because we have good drugs to lower it, but it may not be the real problem. The real problem is low HDL that is caused by insulin resistance (diabesity).
In fact studies show that if you lower the bad (LDL) cholesterol in people with low HDL (good cholesterol) that is a marker of diabesity – the continuum of obesity, prediabetes and diabetes – there’s no benefit. (x)
Most people simply ignore the fact that 50-75 percent of people who have heart attacks have normal cholesterol. (xi) The Honolulu Heart Study showed older patients with lower cholesterol have higher risks of death than those with higher cholesterol. (xii)
Some patients with multiple risk factors, or who have had previous heart attacks do benefit, but when you look closely the results are underwhelming. It’s all in how you spin the numbers. For high-risk males (those who are overweight and have high blood pressure, diabetes, and/or a family history of heart attacks) and are younger than 69 there is some evidence of benefit, but one hundred men would need to be treated to prevent just one heart attack.
That means that 99/100 men who take the drug receive no benefit. Drug ads say the risk is reduced by 33 percent. Sounds good, but that just means the risk of getting a heart attack goes down from 3 percent to 2 percent.
Despite the extensive data showing that statins are a questionable therapy at best, they are still the number one selling drug in the US. What isn’t so well known is that 75 percent of statin prescriptions are written for people who will receive no proven benefit. The cost of these prescriptions? Over $20 billion a year.
Yet somehow the 2004 National Cholesterol Education Program guidelines expanded the previous guidelines to recommend that even more people without heart disease take statins (from 13 million to 40 million) (xiii) What are we thinking?
Why would respected scientists go against the overwhelming research that statins don’t prevent heart disease in people who haven’t already had a heart attack?
You can find the answer if you follow the money. Eight of the nine experts on the panel who developed these guidelines had financial ties to the drug industry. Thirty-four other non-industry affiliated experts sent a petition to protest the recommendations to the National Institutes of Health saying the evidence was weak.
What Should Women Do?
It is time to push the sacred cow of statins overboard.
But first let me say this. If you have had a heart attack, or have heart disease, the evidence shows they do in fact help protect against a second heart attack, so keep taking them. However, you should be aware that most prescriptions for statins are given to healthy people whose cholesterol is a little high. For these folks the risk clearly outweighs the benefit.
The editorial that accompanies the recent study on women taking cholesterol-lowering medication that I opened this article with was quite clear. Dr. Kirsten Johansen from the University of California, San Francisco said that the increased risk of diabetes in women without heart disease has “important implications for the balance of risk and benefit of statins in the setting of primary prevention in which previous meta-analyses show no benefit on all-cause mortality.”
In plain English, she said that we shouldn’t be using statin drugs for women without heart disease because:
- The evidence shows they don’t work to prevent heart attacks if you never had one.
- They significantly increase the risk of diabetes.
Treating risk factors like high cholesterol is misguided. We must treat causes – what we eat, how much we exercise, how we handle stress, our social connections and environmental toxins are all more powerfully linked to creating health and preventing disease than any drug on the market.
Remember what you put at the end of your fork is more powerful than anything you will ever find at the bottom of a pill bottle.
My new book The Blood Sugar Solution, which comes out at the end of February, gives exact details on what you should put at the end of your fork to prevent and reverse diabesity. It provides a comprehensive solution to the health problems facing our nation today.
Now I’d like to hear from you …
What do you think of statins?
Have you taken statins? What has your experience been?
Why do you think the medical establishment prescribes drugs that research shows don’t work?
Please leave your thoughts by adding a comment below – but remember, we can’t offer personal medical advice online, so be sure to limit your comments to those about taking back our health!
To your good health,
Mark Hyman, MD
References:
(i) Abramson J, Wright JM. Are lipid-lowering guidelines evidence-based? Lancet. 2007 Jan 20;369(9557):168-9
(ii) Sirvent P, Mercier J, Lacampagne A. New insights into mechanisms of statin-associated myotoxicity. Curr Opin Pharmacol. 2008 Jun;8(3):333-8.
(iii) Kuncl RW. Agents and mechanisms of toxic myopathy. Curr Opin Neurol. 2009 Oct;22(5):506-15. PubMed PMID: 19680127.
(iv) Tsivgoulis G, et. al, Presymptomatic Neuromuscular Disorders Disclosed Following Statin Treatment, Arch Intern Med. 2006;166:1519-1524
(v) Mora S, Ridker PM. Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER)–can C-reactive protein be used to target statin therapy in primary prevention? Am J Cardiol. 2006 Jan 16;97(2A):33A-41A.
(vi) Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ; JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008 Nov 20;359(21):2195-207.
(vii)Abramson J, Wright JM. Are lipid-lowering guidelines evidence-based? Lancet. 2007 Jan 20;369(9557):168-9
(viii) IBID
(ix) Brown BG, Taylor AJ Does ENHANCE Diminish Confidence in Lowering LDL or in Ezetimibe? Engl J Med 358:1504, April 3, 2008 Editorial
(x) Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJ, Bittner V, Fruchart JC; Treating to New Targets Investigators. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007 Sep 27;357(13):1301-10.
(xi) Hansson GK Inflammation, Atherosclerosis, and Coronary Artery Disease N Engl J Med 352:1685, April 21, 2005
(xii) Schatz IJ, Masaki K, Yano K, Chen R, Rodriguez BL, Curb JD. Cholesterol and all-cause mortality in elderly people from the Honolulu Heart Program: a cohort study. Lancet. 2001 Aug 4;358(9279):351-5.
(xiii) http://www.nhlbi.nih.gov/about/ncep/index.htm
Related Longevity Articles
-

-

-
 6 min read
6 min readUnlocking the Secrets of Resistant Starch for Health and Longevity
Diet & Nutrition Longevity -

-

-

-
 8 min read
8 min readFresh Starts and Fast Results: Your 10-Day Plan for the New Year
Diet & Nutrition Longevity -
 9 min read
9 min readAmerica’s New Dietary Guidelines Get the Big Picture Right—and That’s a Big Deal
Diet & Nutrition Longevity
Women’s Health Support
-
Wellness Essentials® Women's Daily Packs
Regular price $74.95Regular priceUnit price / per -
Wellness Essentials® Women's Prime Daily Packs
Regular price $83.95 / 30 packetsRegular priceUnit price / per -
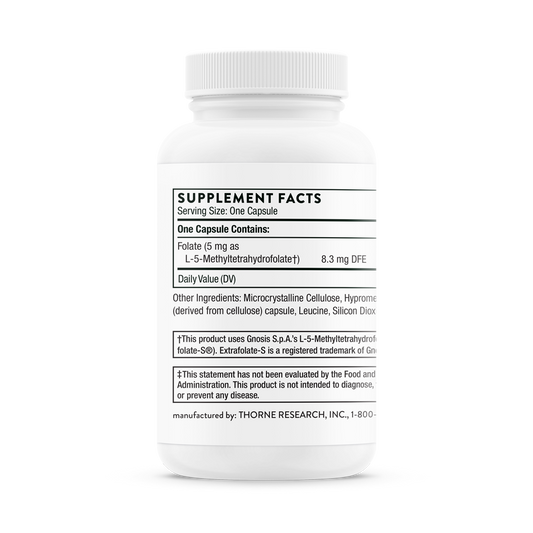
5-MTHF 5mg
Regular price $68.00 / 60 CapsulesRegular priceUnit price / per -
Acetyl-L-Carnitine 500mg
Regular price $80.00 / 60 capsulesRegular priceUnit price / per -
Basic Prenatal
Regular price $37.00 / 90 CapsulesRegular priceUnit price / per -
Bioactive Collagen Complex Daily Foundational Support
Regular price $59.00 / 13.9 oz PowderRegular priceUnit price / per -
Biotin 8mg
Regular price $26.50 / 120 CapsulesRegular priceUnit price / per -
Black Cohosh Plus
Regular price $49.95 / 60 TabletsRegular priceUnit price / per -
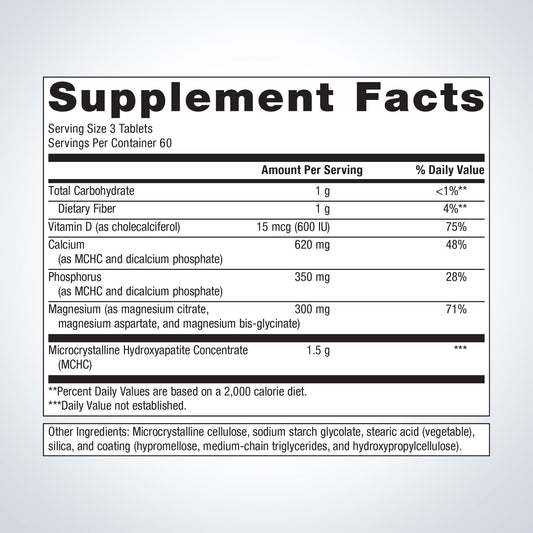
Bone Builder Chewable
Regular price $35.95 / 90 Chewable TabletsRegular priceUnit price / per -
Bone Builder with Magnesium ( Formally Cal Apatite Bone Builder with Magnesium)
Regular price $66.95 / 180 TabletsRegular priceUnit price / per -
Boron Glycinate: 2 mg
Regular price $14.00Regular priceUnit price / per -
Calcium-d-Glucarate
Regular price $79.00 / 60 CapsulesRegular priceUnit price / per
Login
- Choosing a selection results in a full page refresh.
- Opens in a new window.